Bedsores: Causes, Staging and Treatment
Bedsores, also called pressure ulcers or pressure sores, are injuries to the skin and underlying tissue due to prolonged body pressure. They most commonly occur on or around the bony areas of the body, such as the hips and tailbone; they may also occur on the heels and ankles.
These sores can develop surprisingly fast and put patients at risk for dangerous secondary complications, such as infection or permanent tissue damage. They also can progress quickly if not properly treated, particularly in people with compromised immune systems or other underlying medical problems.
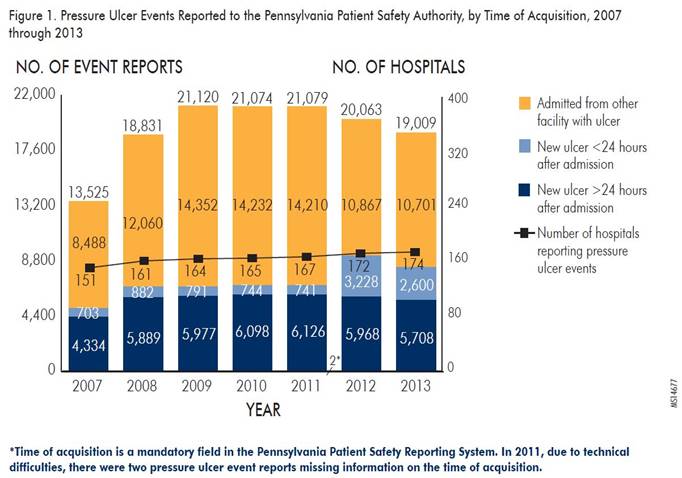
Bedsores afflict patients of all ages, ethnicities, and genders. Around 10 percent of nursing home residents had at least one bedsore in 2004, the most recent year the Centers for Disease Control and Prevention recorded national estimates. Bedsores affect up to 3 million adults annually throughout the United States, causing $11 billion in health care costs and leading to 60,000 deaths yearly. People with medical conditions that limit their ability to move and change positions and those who remain confined to a bed or wheelchair for long periods are at the greatest risk.
What Causes Bedsores?
The application of prolonged pressure reduces blood flow to the body’s tissues and set off a cascade of biochemical reactions that lead to inflammation and bruising. These physical insults then test the immune system and create opportunities for infection.
The body is designed to move and experience shifting, dynamic forces. When a person is very sedentary for a prolonged time – for instance, when her bones push against a surface, such as a bed or chair, for days at a time – the skin constricts and starves underlying tissue of oxygen.
Other physical forces can then worsen the situation. For instance:
- Friction. Movement abrades the skin, for instance, when a caregiver changes a patient’s position in bed or transfers him. Moist or fragile skin is particularly vulnerable to frictional injury.
- Shear. Opposing external forces can exert pressure on the body, damaging blood vessels and creating tearing injuries at both microscopic and larger scales. When hospital beds move up and down, for instance, patients sliding in bed can suffer shearing damage.
Who Is at Highest Risk?
Anyone with limited mobility can develop pressure ulcers, but patients who are confined to their bed, whether suffering from an age-related condition or recovering from an injury, face special vulnerabilities. Other specific risk factors include:
- Age. Skin gets more fragile with age, making the elderly more susceptible to tissue damage.
- Malnutrition. Poor nutrition and a lack of hydration can damage the skin and hamper the body’s ability to withstand the insults of extreme sedentary behavior.
- Medical conditions. Certain illnesses – especially those that restrict blood flow and compromise the immune system – increase risk.
- Smoking. Smoking affects your circulation and keeps necessary nutrients from reaching tissues. Patients who smoke – as well as those who used to smoke heavily in the recent past – are generally more susceptible to developing pressure ulcers.
- Muscle spasms. Uncontrolled body movements such as spasms put patients at higher risk for shearing.
- Bowel incontinence. Excessive moisture and bacteria from fecal matter can lead to localized infections and friction sores.
- Sensory perception. Some brain and spinal cord injuries result in damaged sensory perception, which may impair a patient’s ability to perceive discomfort. Patients who struggle with sensory perception may not be aware of the need to change positions.
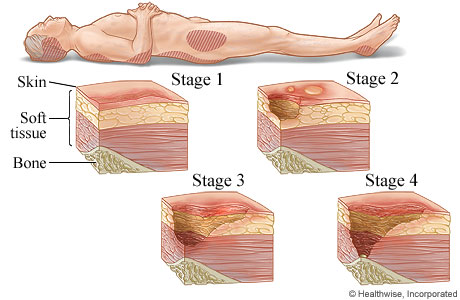
Classifications of Bedsores
The main symptoms of bedsores are pain related, but physicians classify bedsores based on many clinical symptoms. There are four different classifications of bedsores:
- Stage I bedsores do not feature broken skin, but the tissue appears red or purple. It will not lighten to the touch. The site is often painful, firm, tender, and soft compared to the surrounding tissue.
- Stage II bedsores have damaged epidermis (the outermost layer of the skin). The resulting wound is shallow, and it may be red, closely resembling a fluid-filled or ruptured blister.
- Stage III bedsores affect the underlying layers of skin and usually expose the fat beneath it. The wound may appear crater-like and have a yellowish appearance from dead tissue.
- Stage IV bedsores are the most serious, and they may expose muscle or bone. The wound is gaping, and it will have yellowish or dark crusty skin surrounding it.
Potential Complications From Bedsores
Bedsores can be mild to advanced and can have serious complications. Patients may develop sepsis, which is a life-threatening emergency that can lead to multisystem organ failure. Cellulitis and bone infections are other possible complications. Untreated bedsores can lead to squamous cell carcinoma in rare cases, an aggressive type of cancer that usually requires surgery.
Treatment of Bedsores
The incidence of bedsores ranges from 0.4 percent to 38 percent in hospitals, from 2.2 percent to 23.9 percent in skilled nursing facilities, and from 0 percent to 17 percent for home health agencies according to the National Pressure Ulcer Advisory Panel (NPUAP). Stage I and Stage II bedsores will usually heal on their own with little intervention and conservative treatments. Reducing pressure to the area is the first step in treating minor ulcers. Caregivers should reposition their patients frequently – every 15 minutes is ideal during the treatment process.
Stage III and IV ulcers are more difficult to treat, and treatment focuses on managing pain and preventing infection.
- Regularly cleaning and dressing the wound. Stage I bedsores only need to be cleaned with mild soap and warm water. Ulcers with broken skin can be washed with a saline solution at each dressing change.
- Debriding. Wounds must be clear of dead and infected tissue to heal. Removing this tissue is called debridement. There are several different forms of debridement, and a treatment team will select the appropriate type based on staging, severity, and wound location.
- Wound Vac. A wound VAC is often used when the tissue isn’t healing as quickly as it should or when the skin i around the sore isn’t healthy. The wound VAC has sponges that you put on or inside your wound to bring in blood to keep the tissue healthy.
- Antibiotics (either topical or oral) are useful for treating bacterial infections involving bedsores.
- Severe bedsores may require surgical intervention to improve the wounds’ condition. The primary surgery is called flap reconstruction. This is where a part of the patient’s muscle, skin, or other tissue is used to cover the wound and cushion the exposed bone.
Preventing Bedsores
Once they reach a certain severity, some bedsores may never fully heal. Fortunately, caregivers can take steps to prevent them from occurring. Proper bed sore policy and management are essential for nursing and long term care.
- Surface: Make sure patients have the right support. Use special pads or air mattress to relieve pressure at bony points.
- Skin inspection: Early detection helps prevent both bedsores and subsequent infection. If the skin is dry and cracking this may be the early signs of a sore.
- Keep patients moving: Reposition bedridden patients frequently. Nursing homes are typically required to turn patients every 2 hours.
- Incontinence: Keep patients dry and clean. If a patient uses depends or similar product it should be replaced every time it is soiled.
- Nutrition and hydration: The right balance of nutrients and water keeps oxygen flowing to the tissues throughout the body.
Caregivers and practitioners must take appropriate steps to avoid infection and other complications in bedsore patients. If you have concerns about one of your family member’s treatment in a nursing home, please contact us for a free consultation at 1-800-7-legal-7.
Sources:
http://www.mayoclinic.org/diseases-conditions/bedsores/basics/treatment/con-20030848
https://www.ncbi.nlm.nih.gov/books/NBK2650/